When a patient goes into cardiac arrest in a hospital or other critical care setting, their survival depends on the swift response of medical staff trained in cardiopulmonary resuscitation (CPR). As leaders in CPR training for healthcare providers, CPR Tampa understands the vital role of proper CPR techniques and protocols in these high-stress scenarios. This article will examine CPR in emergency rooms and intensive care units, real-life case studies, and the importance of ongoing training and practice.
The Critical Role of CPR in Emergency Rooms
The emergency room (ER) functions as the frontline of any hospital's critical care services. Patients arrive in highly unstable conditions, ranging from trauma to cardiac events and drug overdoses. ER staff must quickly assess and stabilize patients who are often teetering on the edge of life and death.
For patients arriving in cardiac arrest or who lose a pulse during treatment, immediate CPR can spell the difference between death and survival. According to the American Heart Association (AHA), patients in cardiac arrest have just a 10% chance of survival. High-quality CPR can double or triple those odds.
ER teams are trained to initiate continuous chest compressions within 10 seconds of a cardiac event. Research shows even short interruptions in compressions drastically reduce blood flow to vital organs. ER staff are also trained to integrate airway management, rescue breathing, defibrillation, and medication delivery while maintaining constant compressions.
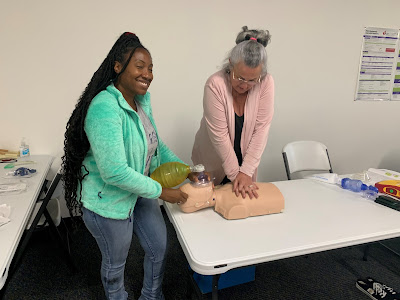
These protocols require extensive initial training and frequent practice in CPR Tampa classes to keep skills sharp. Chest compression depth and rate, synchronizing compressions with ventilations, and smooth hand-offs between providers doing compressions are all critical to maximizing perfusion during CPR.
Maintaining CPR Excellence in Intensive Care Units
Intensive care units (ICUs) treat the most critically ill patients who require constant monitoring and intensive therapies. Patients in ICUs depend on machines and medication drips to support their compromised respiratory, cardiac, and other bodily functions.
A major part of an ICU nurse's job is continually assessing a patient's readiness for liberation from mechanical ventilation. If a patient shows signs of declining oxygen levels or heart rhythm instability when removed from a ventilator, nurses must act quickly to restart ventilation and begin CPR if needed.
ICU teams have specialized resources to optimize CPR for patients already connected to advanced monitoring and therapeutic machines. Portable ultrasound helps guide proper hand placement and depth during compressions. Capnography monitors ventilation effectiveness by measuring carbon dioxide output.
Extra staff allow rotating compressors to avoid fatigue over prolonged codes. ICU nurses train to smoothly take over ventilations, cardioversion, epinephrine administration, and other interventions while keeping up continuous high-quality chest compressions.
Real-Life Examples of CPR Determining Life or Death
The true impact of top-notch acute care CPR skills comes into stark focus when looking at real-life examples.
A middle-aged man arrived at an ER in full cardiac arrest after the fast deterioration of his chronic lung disease. ER staff immediately started chest compressions and put on a LUCAS mechanical compression device to maintain consistent depth and rate of compressions. This allowed the team to better focus on airway intervention and timely defibrillation. The patient revived after 10 minutes and made a full recovery.
In another case, a 59-year-old woman on a ventilator in the ICU suffered a myocardial infarction and lost her pulse. The ICU team initiated CPR with efficient coordination between chest compressions, bag ventilation, and medication administration. They were able to restore circulation after 15 minutes and place an emergency percutaneous coronary intervention (PCI) to reopen the blocked heart vessel.
These dramatic cases clearly demonstrate how proper CPR training and vigilance lead directly to saving lives in critical healthcare settings. The CPR Tampa experts provide the depth of knowledge and hands-on skills practice to empower healthcare teams for such high-stakes scenarios.
Invest in Your Healthcare Team's CPR Readiness
Any links in the patient care chain depend on each provider's ability to execute proper CPR techniques. As a healthcare administrator, ensuring your ER, ICU, and general staff maintain sharp CPR skills should be a top priority.
CPR Tampa offers American Heart Association-certified courses tailored for different experience levels and specialties. From basic life support (BLS) for the general provider to advanced cardiovascular life support (ACLS) for veteran acute care teams, the CPR Tampa courses will hone the speed and coordination needed for real-life codes.
Ongoing skills practice and updated training every two years provide assurance to patients, families, and the community that your facility's teams are true lifesavers ready for the most critical events. Contact CPR Tampa today to schedule consultations on leveraging our AHA training programs. Invest in your staff and invest in saving lives!
Ready to equip your healthcare teams with acute care CPR mastery? Contact CPR Tampa today to learn more about our American Heart Association certification courses!
Comments
Post a Comment